Please click here to download PDF slides:
Cardiovascular System Slideshow PDF
The Cardiovascular System
The body possesses an elaborate system to deliver oxygen and nutrients to cells on its surface and deep within its core. This delivery system is the cardiovascular system.
Its important functions are:
- Supplying oxygen from the lungs to the tissues
- Supplying substances absorbed from the digestive system to the tissues
- Removing carbon dioxide from the tissues to the lungs
- Removing waste products from the tissues to the kidneys
- Regulating body temperature; increasing the diameter of blood vessels increases heat loss, whereas reducing the diameter of the blood vessels prevents heat loss
- Distributing hormones and other chemicals to different parts of the body
The Heart
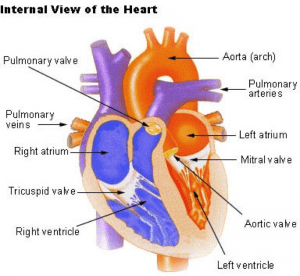
The heart is located between the lungs in the middle of the chest, immediately behind and slightly to the left of the breastbone (sternum). In the front, the heart is protected by the breastbone, in the back by the spinal column and on the sides by the ribs. It weighs 7-15 ounces and is about the size of a human fist.
We have two circulatory systems; the systemic and the pulmonary. The systemic system feeds the organs, tissues, and cells of the body. Fresh oxygenated blood is pumped through the arteries and deoxygenated blood returns to the heart through the veins.
The pulmonary system is just doing the opposite. Deoxygenated blood is pumped out of the heart through the pulmonary arteries into the lungs, and recharged, oxygenated blood returns to the heart through the veins. It is this recharged, oxygenated blood gets pumped out through the systemic circulatory system. These two separate systems must be perfectly balanced in terms of input and output.
With each beat, the heart muscle expands and contracts, sending 2 to 3 ounces of blood on its way through the vascular system. The full circuit around the lungs only takes about one minute to complete when the body is at rest. In that same minute, the heart can pump in the average human 7,5 liters (ca.2,000 gallons) of blood to every cell in the body.
Blood vessels
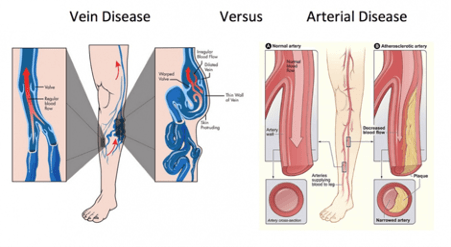
Arteries are blood vessels, which, carry oxygen-rich blood away from the heart to the various tissues in the body. The walls of arteries are lined with smooth cells (endothelium). Around this is elastic tissue and muscle.
The arteries of the body split up into successively narrower branches, until they form the very fine (microscopic) capillaries.
Capillaries have very thin walls and allow the exchange of substances between body cells and the blood.
Several capillaries join to form successively wider branches, ultimately form a vein. Veins carry oxygen–depleted blood back to the heart.
Veins have significantly thinner walls compared to arteries. They are provided with valves, which allow the blood to only flow in one direction – towards the heart.
An average adult has 4.7 to 5.6 liters (5 to 6 quarts) of blood, which is made up of 55% plasma and 45 % cells (red blood cells, white blood cells and platelets). In addition to blood, the circulatory system moves lymph, which is a clear fluid that helps rid the body of unwanted material.
Red Blood Cells
- Carry oxygen from the lungs to all cells in the body
- Carry carbon dioxide from the cells back to the lungs to be exhaled
- Are filled with hemoglobin, an iron-containing molecule that gives blood its red colour.
White Blood Cells
- Protect the body against bacteria, viruses, or other foreign cells
- Are manufactured and stored in bone marrow until needed by the body
- The body produces more white cells when needed to fight infection
Platelets
- Help repair damaged vessels
- Stop the bleeding and harden into a patch over a damaged area of a blood vessel
Blood is ejected from the left ventricle through the aorta. This large artery (2.5cm in diameter in the adult) has numerous branches, so that the oxygenated blood reaches the different parts of the body.
Whenever blood flows through an artery, its flexible wall expands at each heartbeat and this can be felt as the pulse, by passing a superficial artery gently against the bone beneath.
The pulse is usually taken at the wrist, where an artery (the radial artery) passes over the bone.
The blood also exerts pressure on the vessel walls as it is pumped through. Pressure is necessary for circulation to take place. The pressure has a rhythmic fluctuation-the pressure is maximum during systole or when the ventricles are contracting. It is least when the ventricles are relaxed- in the diastolic phase.
The blood pressure hence has two readings –the systolic and diastolic. Blood pressure varies from person to person, as well as from time to time in the same person. It is influenced by many factors such as general health, heredity, age, activity, position of the body and emotional state. The blood pressure is determined by the cardiac output and the peripheral vascular resistance (the diameter of the blood vessels).
Hence, if the heart pumps with force and also at a greater rate, the cardiac output increases, increasing the blood pressure (activities, narrowed arteries)
During the stress response sympathetic nerves increase the rate and force of the heart beat. Sympathetic nerves also cause the arteries supplying the skin to narrow, hence increasing the peripheral resistance. Therefore the stress response which is sympathetic mediated, increases blood pressure.
Blood pressure
A normal young adult may have a Blood Pressure (BP) of 120/80 mmHg, this means that the systolic pressure is 120, while the diastolic is 80.
Considerable variation within the normal range is possible.
A systolic pressure above 140 mm, and a diastolic pressure above 90 mm is considered high blood pressure and needs attendance.
- Your body has many mechanisms for controlling blood pressure.
- It can change the amount of blood the heart pumps by affecting renal water retention and thereby blood volume.
- It can change the diameter of arteries and thereby increase or decrease pressure.
- To increase blood pressure, it can pump more forcefully or more rapidly.
- It can seal off capillaries forcing the blood into a smaller space, thereby increasing pressure.
All of these things happen automatically, regulated by a healthy body, without ever thinking about it. In addition, blood-pressure measurements can vary throughout the day, affected by everything from:
- Alcohol
- Caffeine
- Smoking
- Climate
- Time of day
- Diet
When a healthy diet and lifestyle is not followed, then hardening of the arteries or Atheroma occurs. This happens when inflammation in the lining of the blood vessels causes small areas of damage. Inflammatory cells and cholesterol in the blood, stick to the damaged area to try to repair it. Eventually calcium forms in this plug and build a permanent lump on the side of the blood vessel. This narrows the blood vessels and causes resistance to the flow of blood.
This results in high blood pressure (Hypertension) and blockages, which can cause angina or heart attack in the blood vessels of the heart, a stroke in the blood vessels of the brain and lack of blood flow to other parts of the body.
Angina is where the blockage causes a narrowing of the heart blood vessel and this results in pain when the patient walks or exercises. A heart attack happens when there is complete blockage of the heart blood vessel and this damages the heart muscle.
Causes of Hypertension are:
- Kidney disease
- Hormonal imbalances
- Inflammation of arterial endothelial lining
- Diabetes
- Obesity
- Gene Polymorphism of eNOS, PON-1, MTHFR, MnSOD, ACE, ADIPOQ, PAI-1
- Infections
- Poor dental health
- Obstructive sleep apnea
- Dehydration
- Smoking
- Excess consumption of Caffeine/Alcohol
- Drugs
- Chronic Stress
- Valvular Heart Disease
- Diet
- Pregnancy induced hypertension
- Congenital heart Defects
- Primary Aldosteronism
- High Homocysteine levels
- Heavy metals
- Liver disease
(Further explanations see Truly Heal App - Cardiovascular System)
If left untreated, chronic hypertension can cause:
Damage to the heart muscle because of the extra load it puts on the heart
Kidney damage—which leads to more hypertension, which leads to more kidney damage, etc.
Problems that can occur in veins:
Veins do not have a substantial amount of muscle tissue to contract and squeeze blood along, which means without physical activity to cause the skeletal muscles to squeeze the veins, blood has a tendency to pool and stop flowing in veins—particularly in the legs where gravity works against it. Blood that isn't flowing tends to clot. Overtime blood clots stick together forming very large clots. Large clots that stay in place and block the flow of blood cause phlebitis.
If the clot breaks free and starts traveling through the circulatory system, it's called a thrombus. At whatever point it lodges in a blood vessel and blocks it, it's called an embolism. Clots that break free in the legs are unlikely to be stopped anywhere on their way back to the heart. The first place they are likely to lodge is when the right ventricle of the heart pumps them out into the pulmonary circulatory system on the way to the lungs.
If the clot is fairly small, it will lodge in the lung itself and block the flow of blood to a section of the lung. This is called a pulmonary embolism.
DVT, or deep vein thrombosis, is the term now commonly associated with clots that form as the result of prolonged sitting on an airplane. They tend to break free the next time you start moving again with any vigor. This can be several days or weeks after the plane flight itself, which means many people never connect the two events.
There is one other notable place that clots tend to form. As a result of low blood flow or damaged valves, clots can form in the left atrium of the heart. If the clot forms there, it's already past the pulmonary circulatory system so it can't affect the lungs. Unfortunately, the next stop for the clot is out into the systemic circulatory system, where it has a good chance of being pushed up into the brain causing a stroke.
Medical treatments for vascular problems never address the actual causes.
What is a medical doctor likely to offer?
- Clogged arteries
Modern medicine really only has two approaches.
- Surgically repair the damaged area (bypasses and angioplasties).
- Use drugs to improve the flow of blood through the damaged area and minimize the production of cholesterol, which serves as one of the triggers.
Neither of these approaches, of course, actually deals with the real problem.
2. High blood pressure
When it comes to hypertension, doctors rely almost exclusively on pharmaceutical drugs. The four major classes of drugs are:
- Diuretics, which reduce the volume of fluid in the blood, and therefore reduce the pressure. Unfortunately, side effects can include dizziness, weakness, an increased risk of strokes, and impotence.
- Calcium channel blockers, which work to relax and widen the arteries—thus reducing blood pressure. Then again, a major side effect of channel blockers is a 60% increased risk of heart attack.
- Beta blockers, which work by weakening the heart so it won't pump as strongly, thereby reducing blood pressure. One of the major problems with beta blockers, though, is the increased risk of congestive heart failure.
- ACE inhibitors (the new drugs of choice), which like the calcium channel blockers, also work to relax and widen the arteries. Unfortunately, ACE inhibitors can produce severe allergic reactions, can be deadly to fetuses and children who are breastfeeding, and can cause severe kidney damage. Again, none of these drugs deals with the actual cause of the high blood pressure.
3. Blood Clots
Blood clots (or the fear of blood clots) is treated with blood thinners. The standard is Coumadin (warfarin). Coumadin has serious side effects. It can cause severe internal bleeding that can be life-threatening and even cause death. Aspirin is not a good alternative. It may be beneficial at keeping blood flowing through arteries but studies indicate it has no effect on preventing clots from forming in veins.
Communication between heart and brain and vice versa
There is a dynamic, bidirectional communication between the heart and brain/nervous system influencing reciprocal functions. The heart communicates with the brain in four major ways:
- Neurological communication (nervous system)
- Biochemical communication (hormones)
- Biophysical communication (pulse wave)
- Energetic communication (electromagnetic fields)
Research supports the close relationships between stress, depression, anger, grief and cardiovascular disorders. Anger and hostility are linked to increased incidence of heart attacks in previously healthy people, especially men.
Bereavement is associated with increased cardiovascular risk, particularly in surviving spouses and parents.
Natural Treatments that have direct effect on blood clotting, arterial health and hypertension:
Never forget: The causes need to be addressed otherwise we are simply treating the disease naturally instead with drugs.
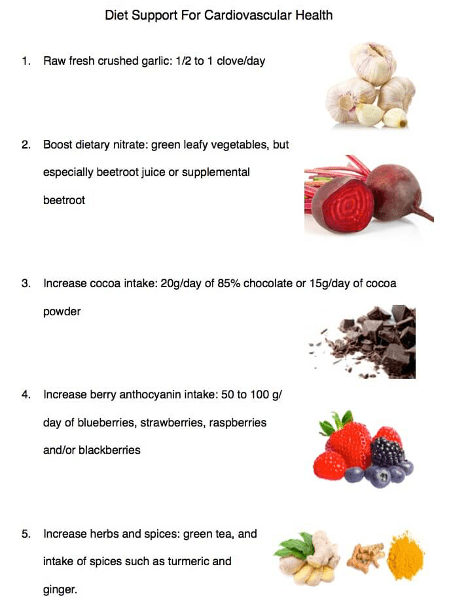
- Studies have shown that dietary changes alone can unplug arteries.
- Proteolytic enzymes, particularly formulas that contain either nattokinase or lumbrokinase, can break down the proteins that hold plaque together stuck to arterial walls—effectively dissolving it.
- Proteolytic enzymes can also help dissolve scarring of the endothelial lining.
Proteolytic formulas that contain seaprose-s, serrapeptase, and/or endonase can help reduce arterial inflammation. - Sufficient Omega-3 fatty acids in the diet also help reduce arterial inflammation and dramatically reduce the circulating levels of damaging NEFAs.
- Antioxidants such as SOD, pomegranate, grape seed extract (AKA OPCs), and pycnogenol help heal the endothelial lining, thereby preventing future plaque and helping to heal current plaque.
- Methylating supplements such as B6, folic acid, B12, TMG, and SAMe help reduce homocysteine levels, thereby reducing damage to the endothelial lining.
- L-arginine and noni extract assist the smooth muscle in arterial walls in obtaining sufficient nitric oxide to function properly.
- Regular heavy metal detoxing can reduce a major cause of irritation to the endothelial lining and a primary instigator of plaque formation.
- Raising body pH through proper diet and the use of supplements reduces lactic acid levels in the arterial smooth muscle, thereby minimizing damage to arterial linings.
- Maintaining a healthy weight
- Stop smoking
- Reducing stress
- Vitamin D, targets many of the factors that contribute to hypertension including suppressing renin and protecting kidney function.
- Magnesium may lower blood pressure both by acting like a natural calcium channel blocker and serving as a cofactor for the production of the vasodilator prostaglandin E1.
- Potassium, the balance of potassium and sodium plays a critical role in blood pressure regulation.
- Vitamin K is known for its ability to reduce vascular calcification and help prevent vascular disease.
- Green Tea Extract has been shown to decrease markers of inflammation and decrease oxidized cholesterol.
- Healthy Diet containing nitrite rich foods, high fiber,
- Garlic, aged garlic has been studied for its ability to reduce inflammation and the damaging effects of cholesterol in the endothelium.
- Ginkgo Biloba favourable alters endothelial function and reduces levels of oxidized LDL.
- Resveratrol benefits the circulatory system by eliciting a decrease in the oxidation of low density lipoprotein LDL;by fostering decreases in platelet aggregation and by promoting relaxation of small blood vessels.
- Quercetin has been found to be a powerful antioxidant and a stimulator of nitric oxide.
- Olive Leaf, the leaves contain the active compounds oleuropein and oleacein, which may function as a vasodilator and ACE inhibitor.
- Omega 3 fatty acids, combat the development and progression of vascular disease via multiple mechanisms including lowering triglycerides, lowering blood pressure, improving endothelial function and raising HDL levels.
- Reducing salt intake
- Oral health
The cholesterol theory
Cholesterol is a compound of the sterol type found in most body tissues. The body and especially the liver make all the cholesterol that is needed and circulates it through the blood.
Over the last 30 years medical professional are telling their patients that high cholesterol is a risk factor for heart disease and stroke. This based on research carried out many years ago.
Finally the research is being re-examined and studied all over again.
- The hypothetical link between high levels of total cholesterol and heart disease has NEVER been proven. It’s a diagnosis conjured up to serve drug companies who want to sell cholesterol-lowering statin drugs.
- Only about 50% of heart attack victims have high cholesterol levels, and 50% of people who have high cholesterol do not have heart disease.
- Chronic inflammation is a major predictor of coronary artery disease. Studies show elevated levels of CRP (inflammation) puts everyone twice at the risk of dying from cardiovascular-related problems as those with high cholesterol.
The benefits of cholesterol are numerous:
- Cholesterol makes hormones, which help to deal with stress and protect against degenerative disease.
- Cholesterol is used to repair damaged cells
- The body needs cholesterol to make all of the sex hormones, including androgen, testosterone, estrogen, progesterone, and DHEA.
- The body uses cholesterol to make vitamin D, vital for the bones, nervous system, proper growth, mineral metabolism, muscle tone, insulin production and regulation, reproduction and immune function.
- Bile salts are made from cholesterol, which is vital for digestion and assimilation of dietary fats.
- Cholesterol acts as an antioxidant, protecting from free radical damage that can lead to degenerative disease.
- Cholesterol is needed for proper function of serotonin receptors in the brain a natural “feel-good” chemical.
Further reading but not required:
Book: The Great Cholesterol Myth
Why Lowering Your Cholesterol Won't Prevent Heart Disease--and the Statin-Free Plan that Will
The best-selling book on heart disease, updated with the latest research and clinical findings on high-fat/ketogenic diets, sugar, genetics, and other factors. Heart disease is the #1 killer. However, traditional heart disease protocols-with their emphasis on lowering cholesterol-have it all wrong. Emerging science is showing that cholesterol levels are a poor predictor of heart disease and that standard prescriptions for lowering it, such as ineffective low-fat/high-carb diets and serious, side-effect-causing statin drugs, obscure the real causes of heart disease. Even doctors at leading institutions have been misled for years based on creative reporting of research results from pharmaceutical companies intent on supporting the $31-billion-a-year cholesterol-lowering drug industry.
The Great Cholesterol Myth reveals the real culprits of heart disease, including: inflammation, fibrinogen, triglycerides, homocysteine, belly fat, triglyceride to HDL ratios, and high glycemic levels. Best-selling health authors Jonny Bowden, PhD, and Stephen Sinatra, MD, give readers a four-part strategy based on the latest studies and clinical findings for effectively preventing, managing, and reversing heart disease, focusing on diet, exercise, supplements, and stress and anger management.
Myths vs. Facts:
Myth: High cholesterol is the cause of heart disease.
Fact: Cholesterol is only a minor player in the cascade of inflammation which is a cause of heart disease.
Myth: Saturated fat is dangerous.
Fact: Saturated fats are not dangerous - the killer fats are the transfats from partially hydrogenated oils.
Myth: The higher the cholesterol, the shorter the lifespan.
Fact: Higher cholesterol protects you from gastrointestinal disease, pulmonary disease, and hemorrhagic stroke.
Myth: High cholesterol is a predictor of heart attack.
Fact: There is no correlation between cholesterol and heart attacks.
Myth: Lowering cholesterol with statin drugs will prolong your life.
Fact: There is no data to show that statins have a significant impact on longevity.
Myth: Statin drugs are safe.
Fact: Statin drugs can be extremely toxic including causing death.
Myth: Statin drugs are useful in men, women, and the elderly.
Fact: Statin drugs do the best job in middle-aged men with coronary disease.
Myth: Statin drugs are useful in middle-aged men with coronary artery disease because of its impact on cholesterol.
Fact: Statin drugs reduce inflammation and improve blood viscosity (thinning blood). Statins are extremely helpful in men with low HDL and coronary artery disease.
About the Authors
Jonny Bowden, PhD, CNS, (Woodland Hills, CA),also known as The Nutrition Myth Buster, is a nationally known, board-certified nutritionist and expert on diet and weight loss. He has appeared on the Dr. Oz Show, Fox News, CNN, MSNBC, ABC, NBC, and CBS and has contributed to articles in the New York Times, Forbes, the Daily Beast, Huffington Post, Vanity Fair Online, Men's Heath, Prevention, and dozens of other print and online publications. He is a popular speaker who presents at both academic and consumer events all over the world.
Stephen Sinatra, M.D., is a board-certified cardiologist, educator, and author who created the Manchester, CT-based Heart MD Institute as an educational platform focused on prevention and proactive lifestyle changes to live a healthier life. He is the author of Reverse Heart Disease Now, The Sinatra Solution, Lower Your Blood Pressure in Eight Weeks, and Heart Sense for Women. He has also contributed to several prestigious peer-reviewed medical journals, including the Journal of the American Medical Association (JAMA), Heart Disease, CT Medicine, and the Journal of Cardiopulmonary Rehabilitation.
For Example: Any Anatomy & Physiology textbook
Book: “Disease Prevention and Treatment” by LifeExtension
