When it comes to gut health there is a common saying:
“You are what you eat”
This saying needs to get chucked out of the window. In actual fact, gut health is actually a lot more complex then this simple phrase. When you look at all the complex chemical and mechanical interactions that happen to get food from one end of the digestive system to the other, the actuality becomes:
“You are what you absorb”
To begin exploring the complicated twists and turns of the digestive system, we must first ask the question; why is our digestive system so important?
Intestinal health is central to our entire health. It is connected to everything that happens in our body.
The health of your gut determines what nutrients are absorbed and what toxins, allergens and microbes are kept out, and therefore it is directly linked to the health of the total organism. Intestinal health could be defined as the optimal digestion, absorption and assimilation of food. But that is a big job that depends on many other factors. For example, the bugs in your gut are like a rainforest, a diverse and interdependent ecosystem. They must be in balance for you to be healthy.
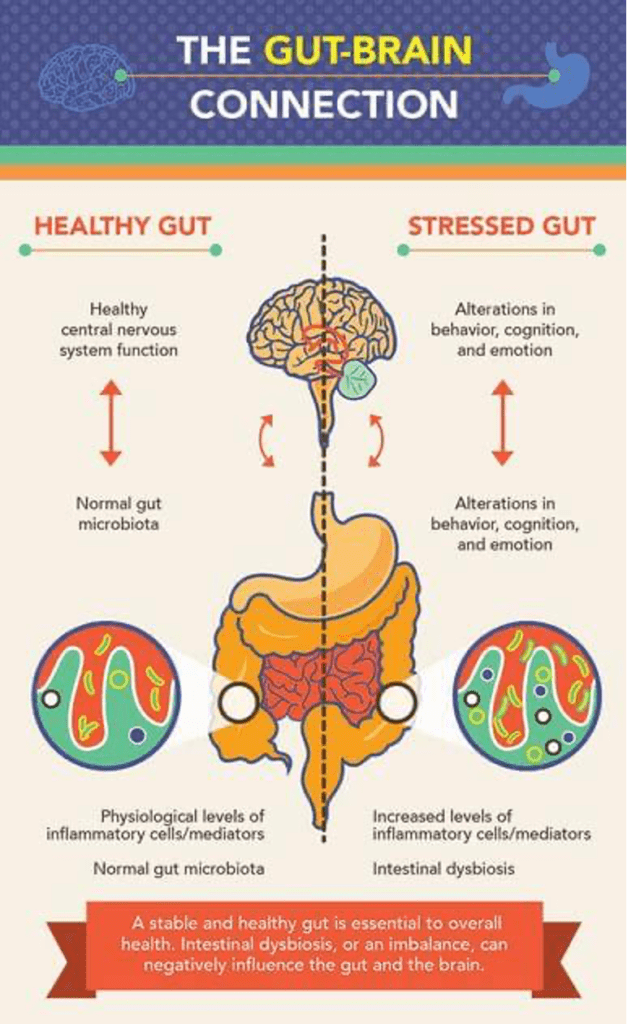
There are 100 million neurons inside the digestive system; that’s more than all the neurons in our peripheries and spinal column. Therefore, our GIT (gastrointestinal tract) is commonly called our second brain. This helps explain why any imbalances in our gut affects our entire system almost instantaneously and why anything that affects our body has a knock-on effect on our GIT. Therefore, the maintenance and integrity of our gut health should be a primary concern to all practitioners.
Bacteria
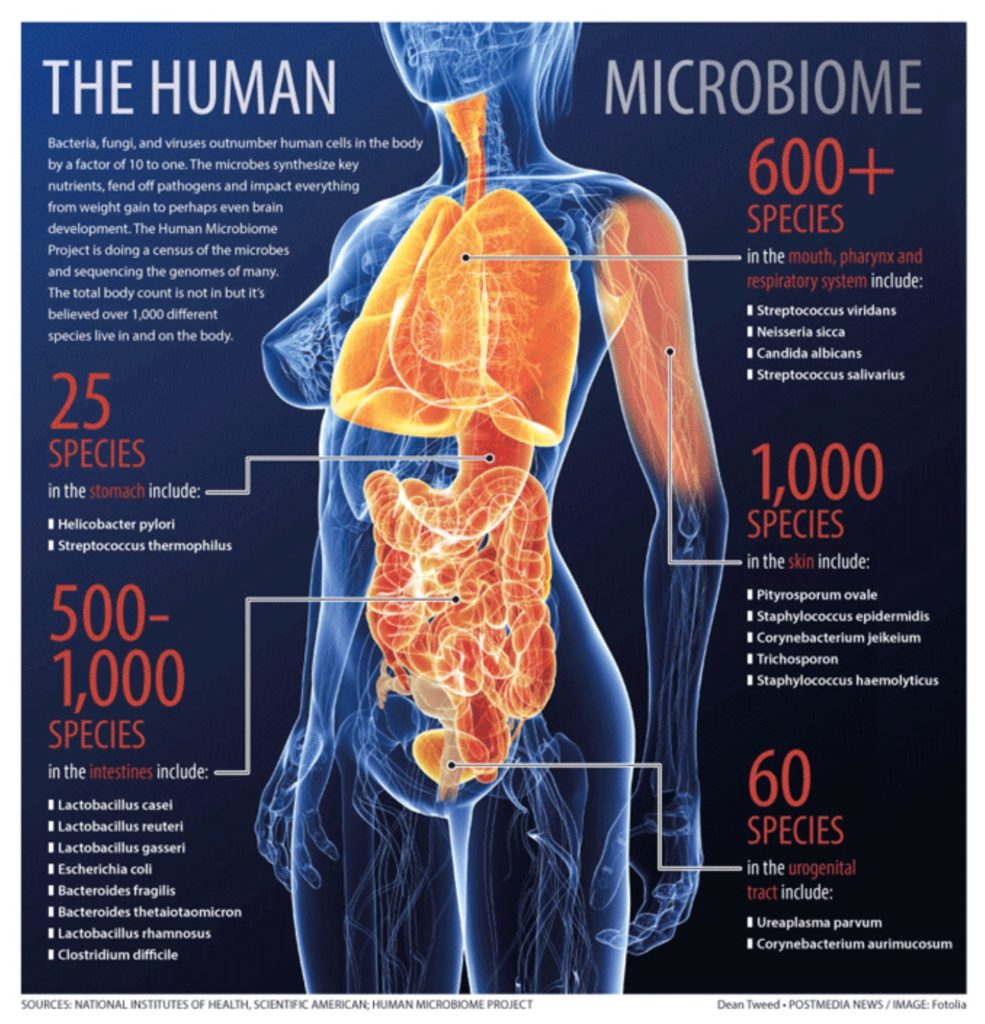
The human body is host to trillions of bacteria. These bacteria play an integral role in our ability to function as a living organism and no living thing can exist without the presence of bacteria. Science is only now beginning to appreciate how big a role bacteria play in everyday health. Bacteria are the basis to our digestive system and are the first line of defence of our immune system.
We have over 1000 different species of bacteria in our GIT, represented by some 5000 distinct material strains. Everyone's gut microbiota is unique, but there are certain combinations and collections of bacteria that are found in healthy individuals. Without them we could not perform functions such as breaking down food, protecting sensitive body tissues and absorbing nutrients. They support our immune system by protecting us from harmful bacteria.
There is a careful balance of good bacteria vs. bad bacteria. Lifestyle and dietary factors affect this balance. The more good bacteria we have, the more powerful our entire body is at absorbing nutrients and fighting of pathogens (bad bacteria).
The day a human is born and removed from the sterile environment in the womb is the first introduction to life enhancing bacteria. As the baby moves through the birth canal, it picks up the mother’s bacteria and later becomes exposed to the bacteria in the mother’s milk. This process is responsible for establishing the baby’s gut bacteria and supporting its immune system. The quality of the bacteria in the birth canal and breast milk is governed by the quality of the bacteria in the mother’s gut. The healthier the bacterial balance of the mother, the greater the chance the baby has for a healthy start.
Therefore, a Cesarean birth (up to 30% in western countries) increases the chance for newborn babies to have a lack of good bacteria introduced into their system from day one.
Pregnant women who suffer from symptoms of fatigue, irritable bowl syndrome and other gut related conditions, need to realise that their gut condition will influence two people instead of one. If the gut has compromised gut bacteria and is malnourished, this will have an effect on the fetus – not only during the gestation period but also from the moment of birth.
Gut bacteria support our immune system and when these bacteria are consistently destroyed our first immune response to disease also gets destroyed. In addition, our digestive functions are also compromised. A lack of nutrient absorption in our digestive system leads to nutrient depleted cells, which eventually leads to disease.
Our good bacteria are killed by a number of toxins and pollutants in the environment and our diet. Some of the most common are: birth control pills, alcohol, stress, antibiotics, high sugar diets, chlorine, fluoride, pesticides, herbicides, etc. Another reason for the death of good bacteria is the overgrowth of bad bacteria. These bacteria can cause many toxic effects and change the entire function of the GIT system.
One of these pathogens is Helicobacter pylori, a bacterium that establishes a life-long infection in humans and is estimated to inhabit the stomach lining of around half the world's population. H. pylori is able to suppress one of the body's natural antimicrobial agents found in the stomach lining which normally helps to stave off bacterial infection. This mechanism could explain why chronic inflammation of the stomach lining is so strongly linked to cancer of the stomach. According to the American Cancer Society, more than half of all cases of stomach cancer are associated with H. pylori infection.
Not having enough good bacteria in the gut can affect the immune system, making it hypersensitive and creating allergic tendencies (hay-fever).
Researchers in Copenhagen reviewed the medical records and stool samples of 411 infants. They found that those who didn’t have diverse colonies of gut bacteria were more likely to develop allergies.
Italian researchers found that between 20 to 75% of patients with chronic fatty liver disease, the kind not associated with alcoholism, also had an overgrowth of gut bacteria. Some believe that the transfer of gut bacteria to the liver could be responsible for chronic liver disease. The liver gets 70% of its blood flow directly from your intestines for first pass metabolism, so the contamination of GIT bacteria into the liver is highly likely.
Two studies from the Mayo Clinic suggest gut bacteria may predict susceptibility to rheumatoid arthritis (RA) as well as offer a possible treatment. A study published online April 21, 2016, by Genome Medicine looked for a biomarker of the disease. Researchers were able to isolate certain bacteria that are high in RA patients, but low in healthy individuals. The other study, published online June 23, 2016, by Arthritis & Rheumatology, found that mice treated with the bacterium Prevotellahisticolahad less severe and less frequent symptoms and fewer inflammatory conditions associated with RA.
A study published online April 13, 2016, by PLOS ONE offered some evidence that a particular strain of the bacterium Lactobacillus johnsoniimay protect against some cancers. Scientists gave mice a mutation that is associated with a high incidence of leukemia, lymphomas, and other cancers. When treated with the bacterium, the mice developed lymphoma only half as quickly compared with a control group.
Research in the February 2016 Journal of Applied Microbiology found the bacterial strain Akkermansia muciniphila could prevent inflammation that contributes to fatty plaque buildup in arteries. Scientists believe the effect was due to a protein that blocks communication between cells in the inner lining of the gut. As a result, fewer toxins from a poor diet could pass into the bloodstream, which in turn reduced inflammation.
The entire immune system (and your body) is protected from the toxic environment in the gut by a layer only one cell thick. This thin layer covers a surface area the size of a tennis court—yet it basically contains a sewer. If that barrier is damaged, the person will get sick and create an overactive immune system, producing inflammation throughout the body.
And then there is the second brain, your gut nervous system. Your gut, in fact, contains more neurotransmitters than your brain. It is highly wired to your brain and messages travel back and forth. When those messages are altered for any reason in any direction – from the brain to the gut or the gut to the brain – your health will suffer.
Main functions of gut flora:
Metabolic
- Fermentation of non-digestible dietary residue and endogenous substances
- Production of mucus
- Saves energy as short-chain fatty acids
- Production of vitamin K
- Absorption of ions.
Trophic
- Control of epithelial cell proliferation and differentiation
- Development and homeostasis of the immune system
- Protection
- Providing vital support for the immune system. Protection against pathogens (the barrier effect).
Antibiotic therapies work by eradicating bacteria (not viruses! A common cold and the flu are caused by a viral infection) This raises a major issue regarding the body's natural microflora. One dose of broad spectrum antibiotics can decrease the gut bacteria by up to 90%! The decolonisation of all internal bacteria raises the chance of harmful bacterial strains recolonising. Dysbiosis commonly occurs post antibiotic therapy. Therefore, the use of antibiotic therapy should be avoided unless absolutely necessary.
Treatment for microflora imbalances must encompass; quality, absorption, location/distribution and the use of specific strains.
Probiotics (live good bacteria) are the called for method of treatment. Probiotics are available as a supplemental form (must not always be refrigerated) and include different strains of bacterium (bifidobacterium, lactobacillus rhamnosus, saccharomyces cerevisiae, etc.). Each strain of bacteria recolonises a different section of the intestinal tract and therefore has specific roles in digestion, immune modulation and intestinal health. Therefore, when combating decolonisation due to antibiotic therapy, a probiotic with a wide range of bacterial strains (lactobacillus=upper GIT, bifidobacterium=lower GIT) is best. However, GIT dysbiosis and disturbances are indicated in almost all disease conditions and the specific supplementation of probiotic strains for this condition has shown to be extremely effective, e.g., lactobacillus rhamnosus gg for eczema and asthma. New studies are constantly being released on this matter. The consultation of these resources for treatment is critical for the most advantageous and clinically relevant support.
In general, probiotics are a supplement which are indicated for a wide range of patients as there is hardly anyone who hasn’t been on several antibiotic treatments in their lifetime.
Some of the functions in probiotics include:
- Regulate peristalsis and bowel movements
- Make necessary vitamins and utilise vitamins B1, B2, B3, B5, B6, B12, A and K
- Digest protein into amino acids
- Breakdown bacterial toxins
- Support immune system and increase number of immune cells
- Balance intestinal pH
- Protect against intestinal toxins.
Recommendation for probiotics:The bacteria count should be in the billion.
When new bacteria are introduced there is a natural die-off period for the bad bacteria and overpowered good ones. This die-off period can cause an initial increase in symptoms, which should be monitored but is not a major concern. The only aid that can be given is ensuring that the patient has a regular bowel movement to aid the clearance of toxins released by dying bacterium. This is most simply and best done with a high plant based diet with adequate hydration.
How to best supplement probiotics is often debated. In the past, the leading theory involved the ‘Weed, Feed and Seed’ method. Weeding referring to the elimination of bad bacteria, feeding referring to the use of ‘pre’ biotics to ensure a fertile and optimistic growing environment, seed referring to the introduction of good probiotic strains.
This theory has been proven to be flawed, causing more damage than good. Weeding is a harsh and often toxic process that has numerous side effects and leaves the body exposed for the proliferation of bad bacteria. ‘Feeding’ only helped to further proliferate the bad bacteria that had grown after the eradication therapy. Finally ‘seeding’ did little to affect the populations of bad bacteria and was considered a waste of money.
New treatment focuses on the crowding out of bad bacteria with good bacterial strains. Therefore, the focus is seed, seed, seed and then feed. This method does not have the negative side effects and returns the body to a natural state of homeostasis without disturbing all other microflora.
Bacteria are living organisms that need to eat. A healthy, varied, balanced, high-fiber diet with complex carbohydrates is good for the bacteria living in your gut and encourages a diverse ecosystem.
Other helpful dietary choices include naturally fermented foods containing probiotics (live bacteria), such as sauerkraut, pickles, miso, certain types of yogurt, and kefir (a yogurt-based drink).
Dysbiosis
The term dysbiosis was originally introduced in the early 1900s by Dr Eli Metchnikoff to describe an imbalance of the bacteria in the gut. Literally it means 'dys' - incorrect and 'biosis' - life. The word comes from 'symbiosis' meaning to reside together harmoniously but with the 'dys' meaning the opposite. He coined the expression ‘Death begins in the gut’.
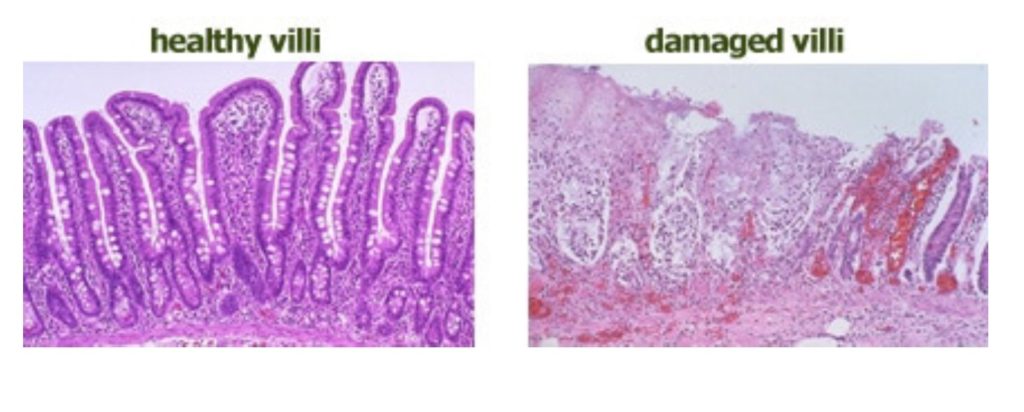
Many microbes are being discovered which should not be located in the gastrointestinal tract and they often release poisonous chemicals such as amines, ammonia, hydrogen sulfide, indoles, phenols and secondary bile acids [2]. These microbes can damage the microvilli in the intestine and can be absorbed into the bloodstream causing a whole range of problems.
Dysbiosis plays a part in many conditions such as irritable bowel syndrome, anklyosing spondylitus, rheumatoid arthritis, inflammatory bowel disease, multiple sclerosis, chronic fatigue, eczema, food allergies, cancer, etc. Many people are unaware that they are even suffering from dysbiosis.
The major causes of intestinal dysbiosis are:
- Stress
- Diets that are quite poor or imbalanced and lacking nutritional supplementation; imbalanced diets may be extreme in carbohydrates, fat, or animal products
- Food allergies or sensitivities (these may in turn be a byproduct of dysbiosis)
- Frequent antibiotic or drug therapy. Antibiotics eradicate any bacteria they come across and this includes the good as well as the bad bacteria throughout the body leaving pathogenic bacteria, viruses and fungi to run free. After each bout of antibiotics a person takes it increases the likelihood that they will develop dysbiosis
- An immune system that is suppressed; this can occur for a number of reasons including emotional stress
- Our low fibre, high sugar, processed food, nutrient poor, high calorie diet that makes all the wrong bacteria and yeast grow in the gut leading to a damaged ecosystem
- Intestinal infections
- Parasite infestation
- Inflammation
- Pesticides, herbcides, fungicides, insecticides. These toxic substances are sprayed on foods that are already nutrient deficient from being grown with artificial fertilisers and are not selective either about which bacteria they kill. They kill the fungal or viral diseases in plants and continue to cause damage throughout our bodies. The pesticides and insecticides used today are often made- up molecules that are awkward for the body to assimilate.
Signs and symptoms of dysbiosis, malabsorption and other GI problems
When the digestive system is out of balance, the following symptoms may occur:
- Bloating, belching, burning, flatulence after meals
- A sense of fullness after eating
- Indigestion, diarrhea, constipation
- Systemic reactions after eating
- Nausea or diarrhea after taking supplements
- Rectal itching
- Weak or cracked fingernails
- Dilated capillaries in the cheeks and nose in the non-alcoholic
- Post-adolescent acne or other skin irritations such as rosacea
- Iron deficiency
- Chronic intestinal infections, parasites, yeast, unfriendly bacteria
- Undigested food in the stool
- Greasy stools
- Skin that’s easily bruised
- Fatigue
- Amenorrhea (absence of menstruation)
- Chronic vaginitis (vaginal irritation).
A new way to fight dysbiosis instead of supplementing with probiotics is fecal transplantation.
A fecal transplant involves inserting stool from a healthy donor into a person's gastrointestinal tract to treat for example recurrent colitis from Clostridium difficile infection. For the procedure, fecal matter is collected from a tested donor, mixed with saline, strained, and then placed into the colon by colonoscopy, endoscopy, sigmoidoscopy, or enema. The longer the patient holds the transplanted stool, the more healthy bacteria are absorbed. A fecal transplant can also be administered in capsule form, or by a tubes going down the nose and into the stomach or small intestine.
A review of existing research in the July 12, 2016, PLOS Biology suggests fecal transplants cure about 90% to 95% of cases of stubborn C. difficile colitis.
Gut Health and Hormonal Balance
Gut health and gut bacteria are the most overlooked elements of hormonal balance (includes menopause, thyroid issues, estrogen excess).
The microbiome is now considered an endocrine organ, some consider it even more powerful than the other endocrine glands – it controls the production and inhibit or support hormonal balance.
- It has been found that the GUT microbiology have an effect not only on breaking down hormones but also in the manufacture of certain hormones, particularly relating to feel good hormone serotonin. In fact the digestive system contains up to 80% of the body’s total serotonin levels. If you are deficient in serotonin then you will become susceptible to depression and mood disorders.
- Gut bacteria impact estrogens by promoting the levels of estriol (the protective estrogen) and helps with reducing symptoms of menopause and osteoporosis.
- They also have an impact on the estrobolome which detoxifies us from the harmful estrogen – these estrogens are the main cause of breast cancers, breast lumps.
- Progesterone is also produced in the micro biome which then signals when and how much to produce.
Leaky Gut Syndrome
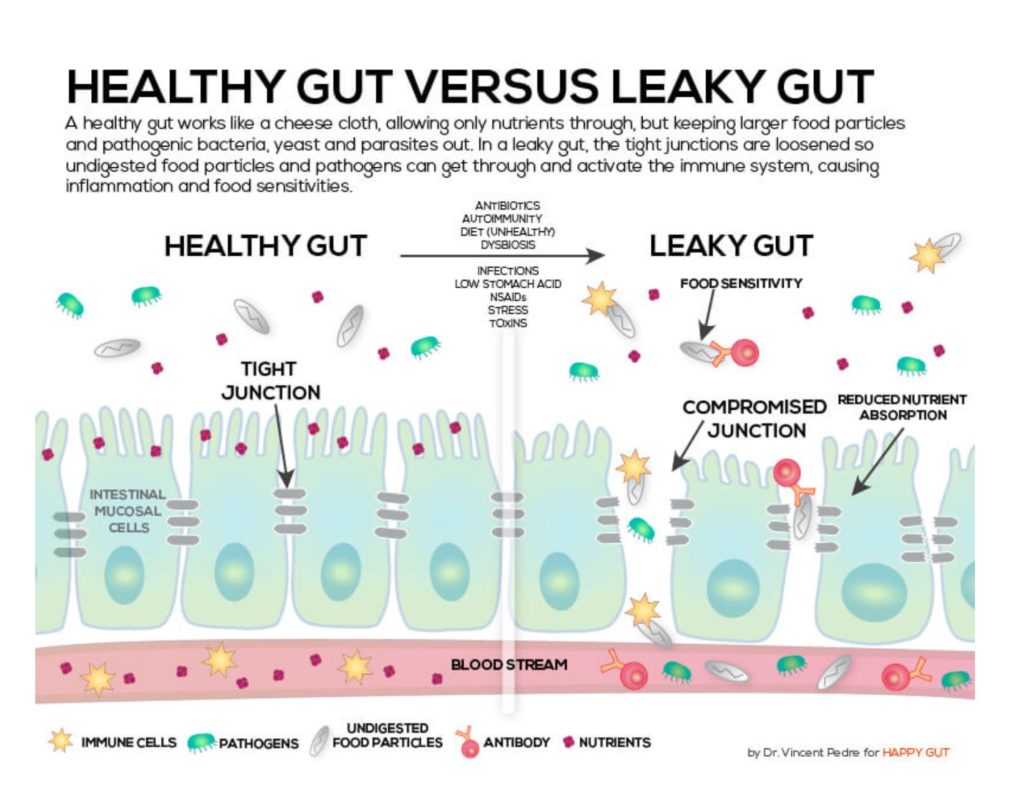
The official definition of leaky gut syndrome is an increase in permeability of the intestinal mucosa to luminal macromolecules, antigens, and toxins associated with inflammatory degenerative and/ or atrophic mucosa or lining.
To explain it more simply, large spaces develop between the cells of the gut wall allowing bacteria, toxins and food to leak into the bloodstream.
In a normal, healthy person the small intestine behaves like a selective sieve, allowing only the breakdown products of digestion into the bloodstream. Nutrients and well-digested fats, proteins and starches are readily able to enter the bloodstream whilst large molecules, microbes and toxins are kept out.
In the intestinal tract, villi (finger-like projections on the lining of the intestinal tract with hair like cell membrane extensions called microvilli) serve as a point of absorption of nutrients. Nutrients such as glucose, amino acids or electrolytes are carried through the microvilli into the cells of the villus via active transport (carrier molecules take the nutrients across the cell membrane).
Leaky gut syndrome causes the intestinal lining to become inflamed and the microvilli to become damaged or altered. The damaged microvilli then cannot produce the necessary enzymes and secretions that are essential for a healthy digestion and the absorption of nutrients.
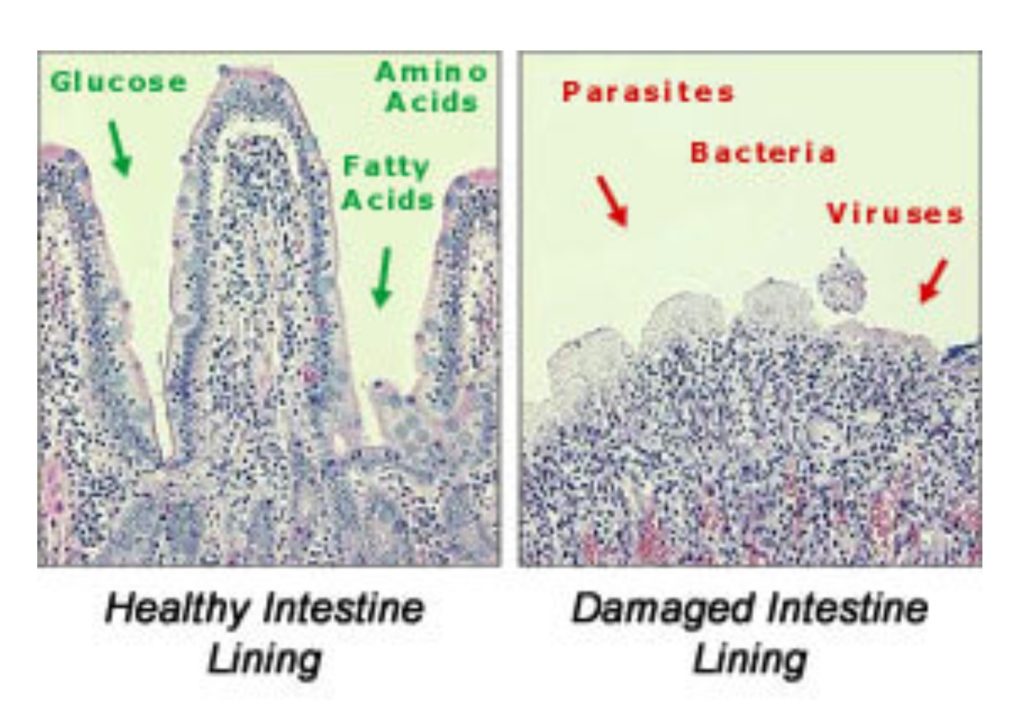
As the damage progresses to the tight junctions, the gaps become wider and wider allowing unwanted particles into the bloodstream. Damage to the intestinal tight junction barrier followed by the invasion of harmful substances leads to inflammation and acts as a trigger for the development of intestinal and systemic diseases as well as overall inflammation.
This provokes the immune system to produce antibodies (a protein utilised by the immune system to locate and attack foreign objects) to fight off the molecules, as they are perceived as antigens (substances capable of triggering the production of antibodies).
A healthy individual would have a strong enough immune system to control the leakage of toxic substances but as it becomes over loaded the toxins leak into the liver resulting in an overworked, overburdened liver.
Causes of leaky gut syndrome:
- Candidiasis
- Dysbiosis
- Alcohol
- Stress
- Food allergies and food sensitivities
- Poor diet
- Celiac disease
- Parasites
- Pharmaceutical drugs
- Exposure to heavy metals.
Symptoms associated with leaky gut:
- Abdominal pain (chronic)
- Insomnia
- Bloating
- Excessive flatulence
- Anaphylactic reactions
- Shortness of breath
- Anxiety
- Fevers of unknown origin
- Gluten intolerance (celiac disease)
- Hemorrhoids
- Heartburn
- Malnutrition
- Migraines
- Muscle cramps
- Multiple chemical sensitivities
- Muscle pain
- Myofascial pain
- Mood swings
- Poor exercise tolerance
- Poor immunity
- Poor memory
- Recurrent bladder infections
- Recurrent vaginal infections
- Recurrent skin rashes
- Brittle nails
- Hair loss
- Swollen lymph glands
- Food allergies
- Constipation
- Diarrhea
- Liver dysfunction
- Brain fatigue
- Abdominal spasms
- Anal irritation
- Constant hunger pains
- Depleted appetite
- Sluggishness
- Depression
- Chronic fatigue.
Conditions that have been linked with leaky gut syndrome:
- Celiac disease
- Multiple sclerosis
- Autism
- Fibromyalgia
- Chronic fatigue syndrome
- Irritable bowel syndrome
- Eczema
- Dermatitis
- Ulcerative colitis
- Candidiasis
- Chronic hepatitis
- Asthma
- Chemotherapy
- Cystic fibrosis
- Multiple chemical sensitivities
- Accelerated aging
- Endotoxemia
- Colon cancer
- Crohn's disease
- Food allergies
- Giardia
- Arthritis
- Pancreatic dysfunction
- Hives
- Acne
- AIDS
- Alcoholism
- Anyklosing spondylitis
- Inflammatory bowel disease
- Liver dysfunction
- Malnutrition
- Psoriasis
- Schizophrenia
- Alcoholism.
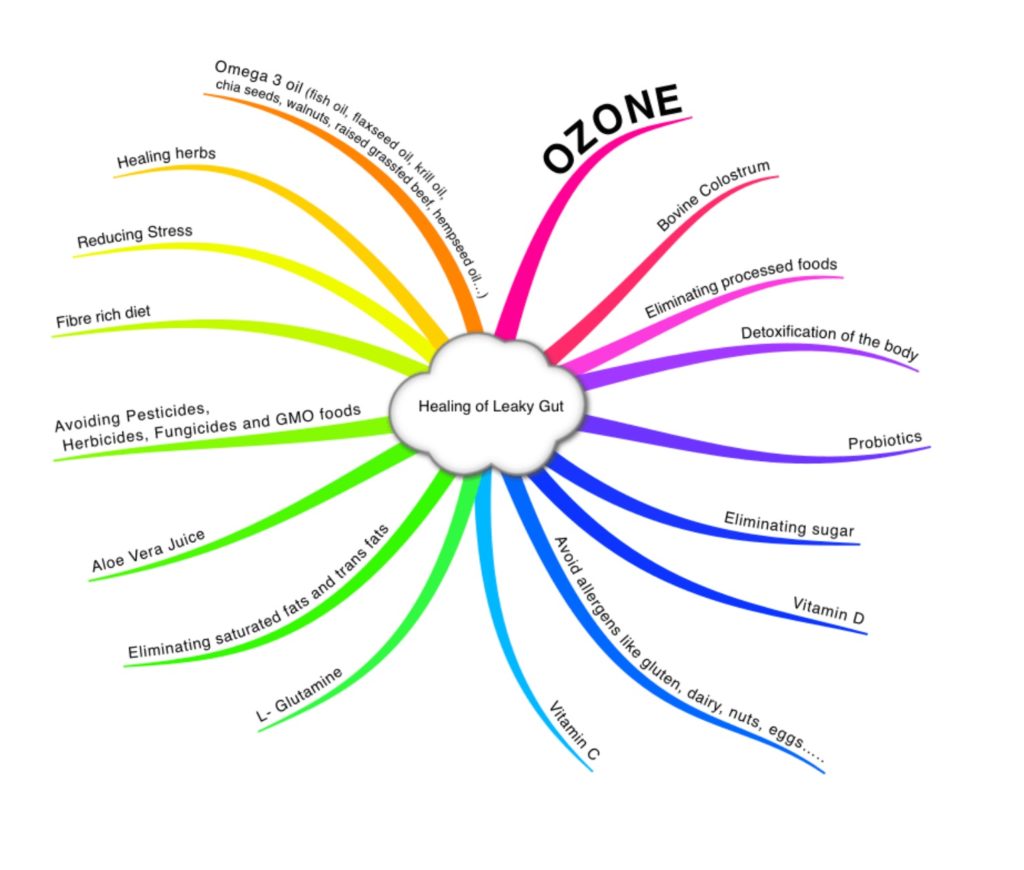
Treatment of Leaky Gut:
- Elimination of food allergens and food sensitivities either through elimination diet or IgG test
- Avoiding dairy and gluten
- Avoiding all processed foods
- Avoiding sugar, alcohol, simple carbohydrates and anything else that lets candida proliferate
- Get plenty of omega 3 fatty acids
- Taking a good probiotic (bacteria count at least in the billion)
- Glutamine is a non-essential amino acid. However, if the immune system is compromised it is said that the body can become deficient. Glutamine is the preferred fuel source for the cells that line the intestinal tract and for the immune system. It has a vital role in cell growth and functions also as an antioxidant. Lymphocytes and macrophages rely on glutamine as an energy source. It has been said that glutamine can speed up recovery of wounds, aid protein metabolism, increase growth hormone levels amongst other healing properties
- Digestive enzymes
- Aloe vera juice has anti-inflammatory properties along with a natural laxative effect to help clear out the bowels. Aloe is known to soothe and cleanse the digestive tract and help improve digestion. It also helps to decrease the amount of unfriendly bacteria in the gut keeping healthy intestinal flora in balance. Aloe is also a vermifuge, which means it helps to rid the body of intestinal worms
- Slippery Elm is used for inflammation and ulceration of the gastrointestinal tract, ulcerative colitis, Crohn’s disease, gastritis, diarrhea, diverticulitis, enteritis, constipation. Slippery Elm needs to be taken with a higher quantity of water to eliminate the risk of constipation.
- Zinc
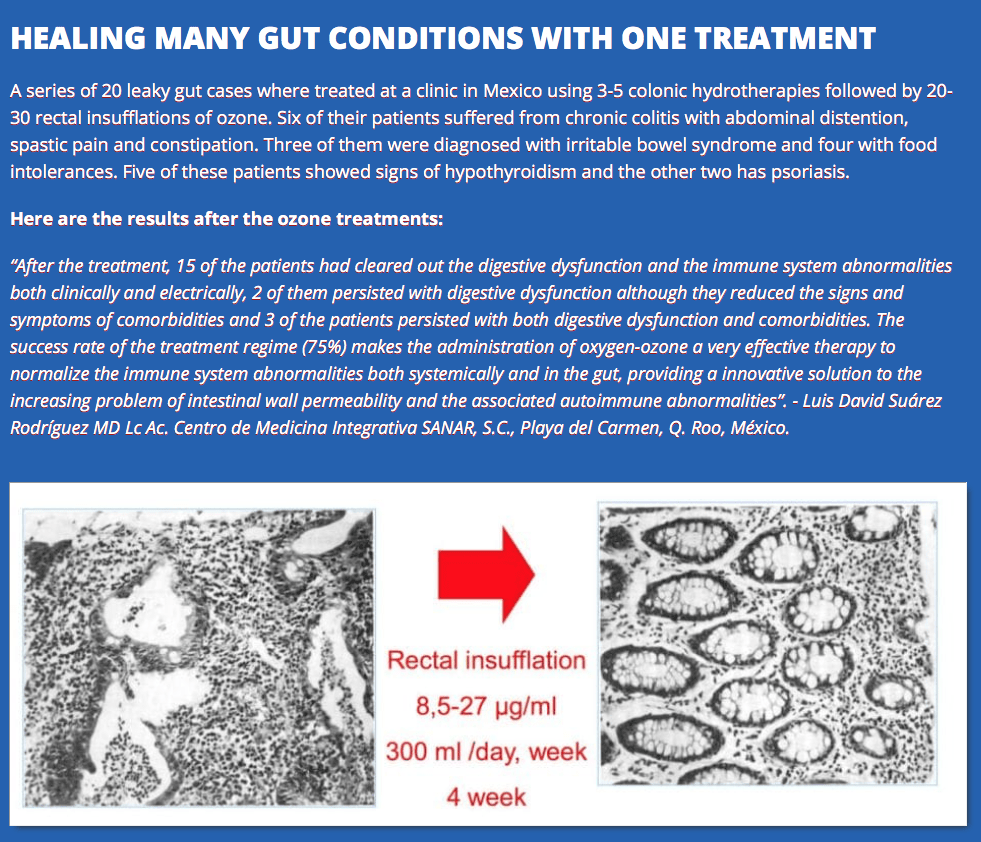
- OZONE
Testing digestive dysfunction:
- Comprehensive digestive stool analysis (CDSA) — available with and without parasitology (Genova, Metametrix)
- Potential laboratory/diagnostic tests for food intolerances/sensitivities (IgG)
- Celiac panel and genetic tests (HLA DQ2, DQ8)
- Organic acids (specifically by-products of gut flora)
- Intestinal permeability testing (lactulose-mannitol)
- Potential laboratory/diagnostic tests for fungal/yeast infections
- Antibody testing (candida, specific moulds, fungi)
- Fungal stool culture and stool smear (false negatives are possible)
- Organic acids: D-arabinitol (false negatives are possible)
- Nasal swab fungal analysis
- Room analysis for moulds and fungi (Petri dish culturing).
Food allergies
Food allergies are a major concern for the entire physical human system. It is one of leading causes of inflammation and free radical damage to organs. Primarily allergic responses cause a direct inflammatory reaction to the cell lining (basolateral border) of the duodenum, jejunum and ileum. Collectively making up the small intestine, this is the primary source of nutrient digestion and absorption. Bile from the liver and pancreatic fluids are released into the small intestine and continue the breakdown of carbohydrates, lipids and proteins into small enough components so they can be absorbed over the basolateral border and absorbed into the bloodstream for first pass metabolism. IgA, IgE and IgG allergic reactions cause the inflammation and eventual degradation of the basolateral border. Perforation of this delicate structure permits the entrance of inflammatory proteins into the bloodstream (leaky gut). These inflammatory proteins result in a multitude of seemingly unconnected/unrelated symptoms.
Symptoms of leaky gut include celiac disease, inflammatory bowel disease (IBD, which includes Crohn’s disease and ulcerative colitis), auto immune diseases, irritable bowel syndrome (IBS), arthritis, psoriasis, eczema, asthma, hives, mental fog, fatigue, joint pain, swelling, arthritis, etc.
The list of conditions that could result from leaky gut is potentially endless due to the system inflammation that is its result.
Along with the inflammatory issue associated with leaky gut, malnutrition becomes an increased threat as the absorption of nutrients becomes disrupted.
Malnutrition
Although allergy born malnutrition is a more common occurrence than most people give it credit for, the leading cause of malnutrition is still due to the SAD diet (Sad American Diet). Firstly, this diet is not in any way exclusive to Americans, it simply refers to the consumption of refined, processed food, high in carbohydrates and fat. These foods are commonly deficient in vitamins, plant phenols and lack a diversity of amino acids, minerals and fatty acids. This diet, although more than plentiful in calories, can cause major nutritional deficiencies in patients. Besides B vitamins, one of the most common deficiencies is omega 3 fatty acids (EPA, DHA). These are powerful anti-inflammatory compounds and, along with cholesterol, make up the fluid lipid bilayer of every cell. Without sufficient omega 3 oils we begin to degrade our membrane potential and increase cellular inflammation.
Medication often attempts to stimulate or suppress the body’s production of a substance. What medicine sometimes fails to realise is that the production and hindrance of organic substances in the body are all produced, modulated and made up of the food that we ingest and absorb. Therefore, a balanced nutritional diet high in fresh nutrients is key to any treatment, medical or alternative.
Gut / Stool Evaluation
To do a proper evaluation of our gut health we have to look at our stool. Frequency, form, smell and color are all important to make a reasonable assessment. If this is also combined with the observation of what food we ate then we can get a proper picture of our digestion and bowel movement. Many people never look at their stool.
Frequency: Generally approved standard would be 1 complete and fully formed bowel movement per day. A gold standard would be 2-3 fully formed bowel movements a day. Going more than 4 times per day is not typically healthy and indicates an overactive digestive system.
Anything less than 1 bowel movement per day would indicate some level of constipation.
Form: To achieve a proper form of stool, our digestive system needs to efficiently break down and assimilate nutrients, as well as passing it through in a reasonable time frame.
With the help of the Bristol Stool Chart we can easily evaluate the best stool forms. Type 3 and 4 are considered healthy.
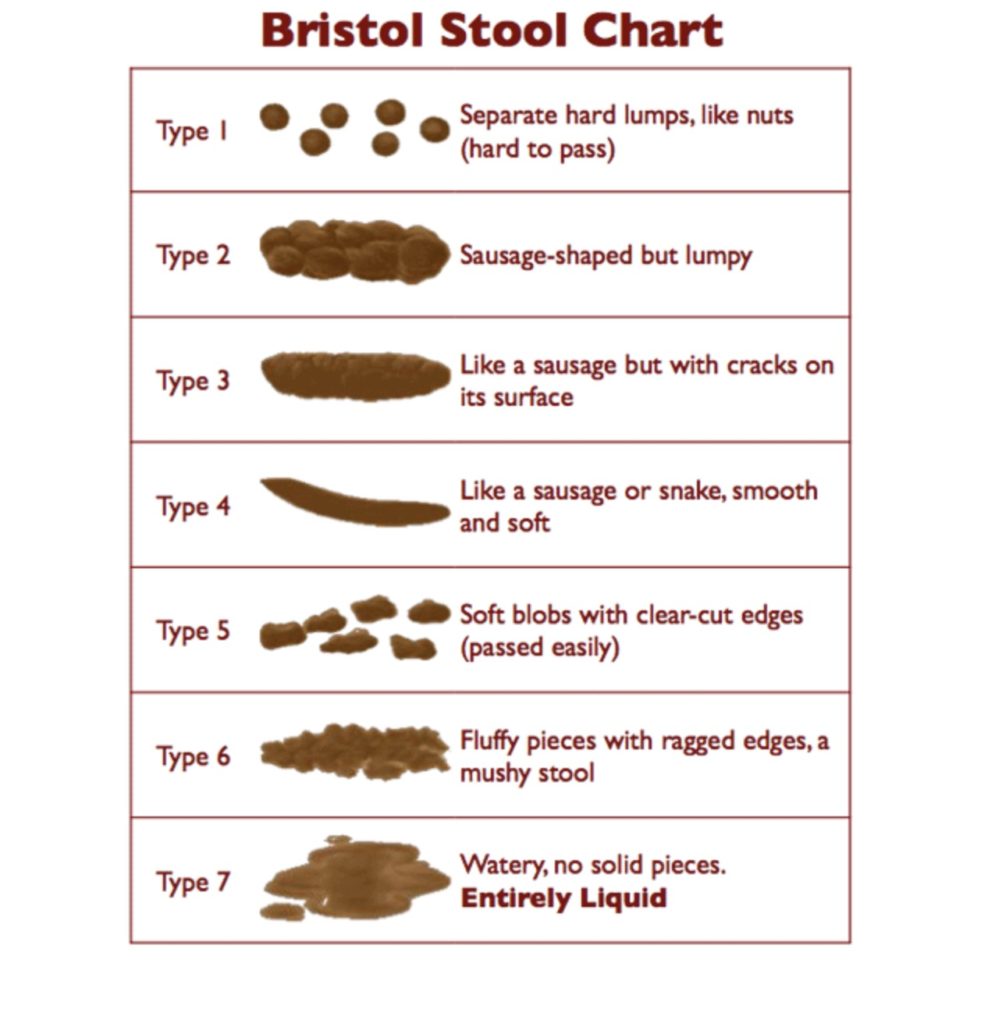
Smell: Every stool smells but if the smell is extraordinarily bad then this can be an indication of a number of digestive problems such as Candida, celiac, and Crohn’s as well as problems such as pancreatitis and liver disease.
Color: An optimal stool is medium to dark brown in color. If it is black, it could be a sign of blood in the upper GI tract. Yellow or green could be a result of fat malabsorption or liver or gall bladder stress. Be aware that certain foods can change the color of stool. Especially dark greens, chlorella, spirulina and beets strongly influence the color.
Indigested food particles: Food particles are a sign of incomplete digestion, which could have several causes.
Mucus: Excessive Mucus is possibly related to IBS, Candida, parasite infection, inflammation.
Download the Diet and Stool Diary pdf for a weekly stool observation.
“Healthy Gut Healthy You”, by Dr. Michael Ruscio
“Gut" the inside story of our body's most under-rated organ by Giulia Enders
Article: Gut Health & The link to Disease
https://www.trulyheal.com/gut-health-the-link-to-disease/
Article: The Gut- Body Connection
Please download the Slideshow PDF file: (big file, takes a bit to download)
Live Webinar 25.03.21 The Gut-Brain Connection
The webinar will start about 40 seconds in.
